Mainstream media is reporting that Mathew Perry died from the acute effects of ketamine after an autopsy report was released on December 12th, 2023. I’m an anesthesiologist of 25 years, published books and SPEAK about mental disease and ketamine. Perry’s death seems straightforward, until you delve into the autopsy report.
First, let’s define the word “acute” —a phenomenon characterized by the sharpness of severity of sudden onset. This means that a cause and effect occur shortly after an event, which in this case is Perry’s acute ketamine administration. On October 28th, 2023, the 54-year-old actor was discovered in face-down his jacuzzi, unresponsive, and declared dead at the scene. The cause of death was reportedly a drowning, and he died sometime between 1137 and 1600 hours.
Mr. Perry, who was open about his lifelong substance abuse struggles, had been receiving regular ketamine infusions for depression and anxiety for some years. His last ketamine treatment was about 10 days before his death and that he’d been reportedly clean for 19 months.
Investigator’s Report
At the bottom of the autopsy report, signed by investigator Jenifer Hertzog lists several prescription and over-the-counter medications found at Perry’s home in Palisades, California on the day of his death – Buprenorphine, Quviviq, Sildenafil (Viagra), cyanocobalamin, Tadalafil (Cialis), Vilazodone, and Minoxidil-Fluocinolone. Notably – there’s no mention of any ketamine of any kind was found on premises, no vials, oral troches, or syringes.
Perry’s lab results are interesting as well. First, it says they were analyzed on November 8th, 10 days after his death. The potassium reads greater than 9 and a glucose of 20, is incompatible with life. These results are typical of a what is called a hemolyzed sample. It’s interesting why they waited so long to run the chemistry panel. Usually, high potassium suggests some type of ischemia, often myocardial.
Buprenorphine
It also states that he was taking buprenorphine (Suboxone) 30 mg for his addiction problems. This is almost the maximum dose except under exceptional circumstances. Perry’s levels were within normal, suggesting that he was taking the medication as prescribed. It’s possible, that this contributed to his death, given that he was on the medication for some time.
Benzodiazepines
The laboratory analysis also states that he was taking Lorazepam, a highly addictive long-acting benzodiazepine for anxiety. A level of 8.4 mg/ml was found in Perry’s blood. This suggests that he took his daily dose of Ativan.
Stomach Analysis
Stomach analysis is important in autopsies because they can indicate the amount of time since death, or if the person ate or not, and if there are medications from an overdose. Perry’s stomach content for ketamine shows about 1mg, which suggests he received a massive dose of ketamine in his blood, and some of it made it into his stomach contents. This pattern is consistent with other overdose deaths from opioids.
Classical pharmacokinetics involves evaluating how a drug is distributed in the body, whether uniformly or non-uniformly. In cases of non-uniform distribution before death, there's a possibility that distribution could become more uniform postmortem due to the flow along concentration gradients, specifically from areas of high concentration to lower concentration, and more generally, along gradients of chemical potential.
Ketamine
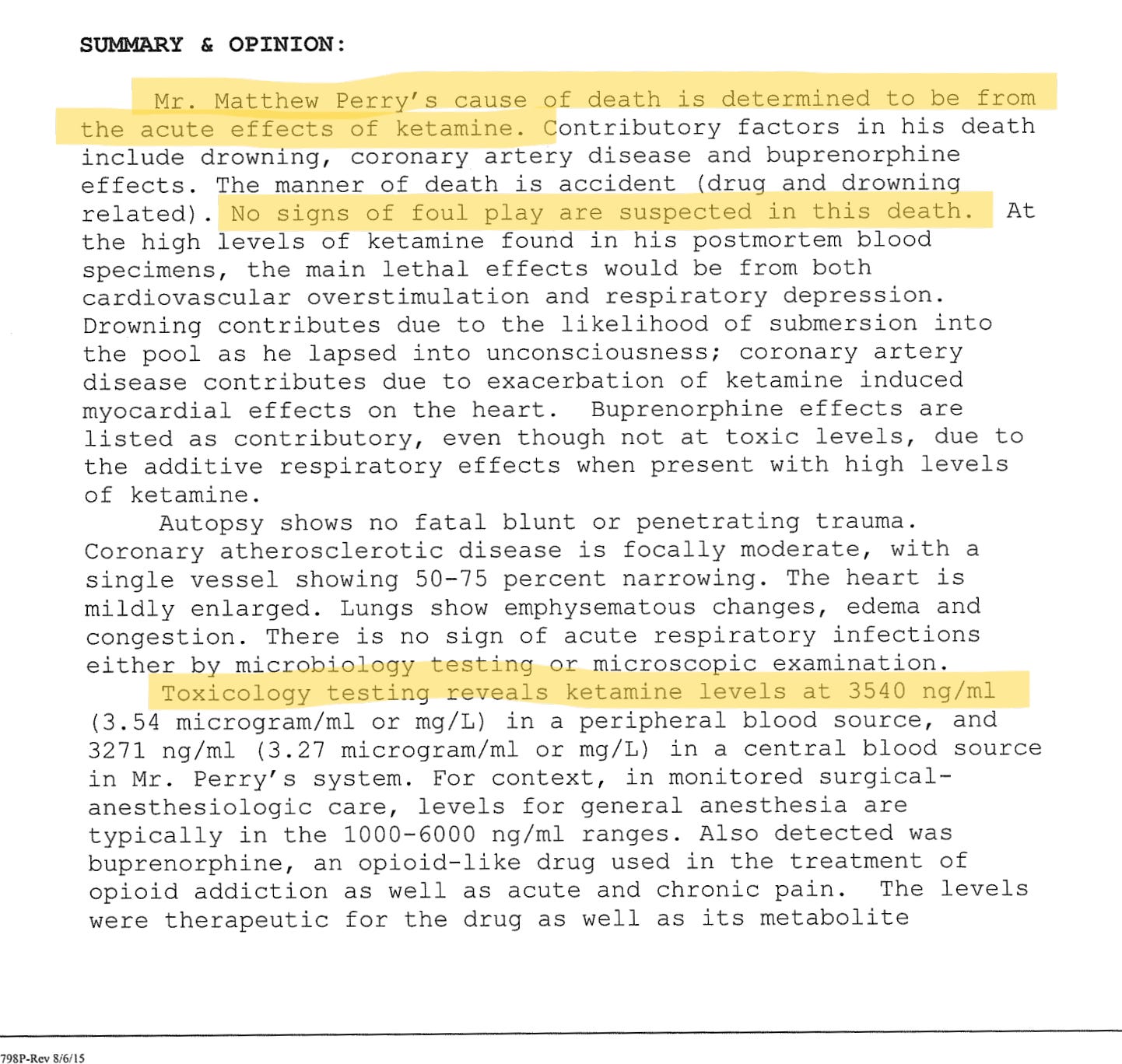
Here’s where the story becomes interesting. Per Perry’s records, he’d been receiving regular ketamine treatments for some time to treat his depression and anxiety. Apparently, it helped as he was out playing pickleball and socializing. His last known ketamine treatment was approximately 10 days before his death; given that ketamine is metabolized in about 2 to 4 hours, it’s impossible this treatment contributed to his death. It’s important to note that most medical examiners never test for ketamine, but they did in Perry’s case, presumably, given his history of ketamine treatments.
Mathew Perry’s ketamine level in his blood was 3500 ng/ml. This is a lot of ketamine. It was said that upon discovering Perry in the water, there were no signs of drugs or other medications. Nor was there a question of alcohol ingestion. The autopsy report specifically stated that there were no signs of an injection from an intravenous catheter or intramuscular injection.
General anesthesia and the major Routes of Ketamine Administration
Anesthesia in humans is typically achieved with ketamine doses of 1 to 2 mg/kg administered intravenously (bolus) or 4–11 mg/kg intramuscularly (reference). To achieve a level of 3500ng/ml, Perry would’ve taken a shit ton of ketamine. He weighs about 100 kilograms (220 pounds). To achieve a level of 3500 ng/ml in his blood, it would’ve taken about 200 to 400 mg of an intravenous bolus of ketamine (meaning giving the ketamine rapidly in one shot). Yet, there’s no evidence of intravenous administration, so we can table that one.
The next route is intramuscular injection. In general, to achieve a level of 3500 ng/ml, he would’ve had to self-inject about 400 to 1100 mg of ketamine. This is an extraordinarily high dose of ketamine for anyone. Let’s assume that he self-injected the ketamine (which is unlikely). Most injectable forms of ketamine come in 50mg or 100 mg per milliliter. This means that he would have needed to inject more than 5 to 10 milliliters into his muscle, which is like injecting an orange under your skin. This is quite a task, even for trained healthcare professionals. If true, then his motives were distant from getting high or having a psychedelic experience. But there weren’t signs of an intramuscular or subcutaneous injection.
Let’s ponder if he took the ketamine orally. Typically, this is done via a troche or sublingual form of ketamine. Since oral administration of ketamine is only about 25% of intravenous administration, it would’ve taken in the order of grams of ketamine to achieve such blood levels. An autopsy should have detected oral ketamine troches. The stomach juices revealed 1 mg of ketamine, as explained earlier. The autopsy report notes that Perry’s assistant was responsible for administering his medications. Additionally, he was under the care of a psychiatrist and anesthesiologist. This says something about Perry’s ability to self-administer medications aren’t likely. At the end of the day, there is only so much gum one can put in their mouth.
Finally, let's consider the intranasal route. After reviewing several studies on the pharmacodynamics of ketamine blood levels following intranasal administration, the suggested level of 3500 ng/ml doesn't seem feasible. While blood levels can indeed become elevated with 9 mg/kg of intranasal ketamine, the upper limits in the studies I've reviewed were less than 2800 ng/ml. Additionally, the authors acknowledged the difficulty in accurate measurement.
Snorting over a gram of intranasal ketamine is an extraordinary feat, if not impossible. Typically, intranasal ketamine vials contain less than 500 to 1000 mg of ketamine. Moreover, intranasal administration can be messy, as the liquid is sprayed into the nostrils, leading to a significant amount of ketamine dripping back down the nasal passages.
The medical examiner stated that Perry died of acute ketamine intoxication. But why not reveal the source of ketamine that should have been found on the premises? This is where the medical examiner’s narrative breaks down.
If Perry did indeed self-administer the ketamine, then he obtained the medication somewhere. And even more pressing, is how did Perry’s blood levels of ketamine come back so high? The fact that there’s no evidence of ketamine injection, or evidence of any type of ketamine at his home, at the time of his death is disparaging. It suggests that someone took the ketamine vial(s) and/or syringes and removed them from the premises. Sadly, it suggests that Perry had ulterior motives of giving himself ketamine.
Heart Attack
The autopsy report also indicates that he had coronary artery disease, contributing to his death. The autopsy revealed blockages of 50 and 75%, respectively, in his most critical coronary artery, the left anterior descending artery, known as the widow-maker. Furthermore, Perry smoked 2 packs of cigarettes daily, had chronic obstructive pulmonary disorder (COPD), was diabetic, and suffered from depression. In addition, he was on Viagra and other medications. On the day he died, he had just finished playing 2 hours of pickleball. If this is not a setup for an acute heart attack, I don’t know what is. No signs of heart muscle ischemia were noted. However, the absence of ischemia doesn’t rule out a heart attack given his multiple risk factors. Perry had plenty of reasons to have a heart attack.
Did Ketamine Give Perry a Heart Attack?
As an anesthesiologist of 25 years, I can tell you that the cardiac effects of ketamine are overblown; even a modest dose mildly increases heart rate and blood pressure. Ketamine stimulates breathing, even at high doses. This is supported by science and my experience in the operating room. Unless Perry was already having a heart attack, then we can consider ketamine causing undue cardiac stress, adding to his death.
Was This an Accident from Ketamine?
This is undoubtedly what the MSM and autopsy report are trying to support. Let’s play devil’s advocate and assume that Perry overdosed on ketamine, had a dissociated state, and fell into the jacuzzi. Definition of dissociative anesthesia—is a form of anesthesia that lacks complete unconsciousness but is characterized by catatonia, catalepsy, and amnesia. Whatever he took rendered him high or incapacitated, and he went into the jacuzzi, swallowed a bunch of water, went into a panic attack, and had a heart attack or something of that nature.
But even so, Perry would have had to inject and/or ingest a very high dose of ketamine to achieve the blood levels he did, render himself in such an incapacitated state, fall into the water, and not care about breathing. When this happens, most people have a strong respiratory reflex that causes them to breathe. In a jacuzzi, he easily could have put his head above water and took a breath. Of course, this is speculation.
Ketamine overdose is a relatively uncommon condition and co-ingestions often complicate severe cases, as in the death of Mathew Perry. Cases of addiction to ketamine are relatively infrequent, and there are scant statistics on relapse rates and prognosis. Nonetheless, ketamine remains one of the few psychoactive drugs with serious complication rates of less than 1%.
In my book, The Revolutionary Ketamine, I write about Edward Domino’s article “Taming the Ketamine Tiger,” which tells the story of the dangers of ketamine. In 1978, Marcia Moore, the wife of an anesthetist, became addicted to ketamine and took the drug daily, which destroyed her sleep architecture. One night, she took ketamine and went outside during the winter. She never returned that night. Two years later, her body was found decomposed in the forest. She likely took enough ketamine, and she succumbed to hypothermia.
The risk of death from accidents when intoxicated with ketamine is associated with the highest mortality rate, according to several studies. One study highlighted two ketamine users died within one year, one from drowning in a bath and the second from hypothermia.
Overall, ketamine is a safe drug. I wrote about this in chapter 9 of my book, The Revolutionary Ketamine. Ketamine’s tolerability and safety have been consistently demonstrated for over 70 years. A review of over 70,000 cases involving ketamine showed that the incidence of complications was extremely low. An extensive body of evidence from operating rooms, sedation procedures, and mental health clinics shows that ketamine is a safe medication. Ketamine is so safe and essential that it’s on the WHO list of essential medications. Also, many criticize that ketamine is often prescribed off-label and does not have FDA approval for mental health disorders. Except for Spravato, more than 50% of mental health medications are prescribed off-label. The same trend is true for other classes of medications.
As an anesthesiologist who’s been giving ketamine in operating rooms, burns units, ICU, and clinic settings for over 20 years, Perry’s story doesn’t make sense. So, what would’ve happened to Perry if it wasn’t for the acute administration of ketamine? Anyone’s guess is as good as mine. We can never know what’s going in someone’s head in these situations.
Mathew Perry’s case is tragic, impacting millions of mental health patients benefiting from proper ketamine treatments. It's a blow to the addicts supported by Mathew Perry's foundation (mathewperryfoundation.org). Some might view it as a win for big pharma companies aiming to promote their depression drugs, or for state and DEA efforts to control and limit ketamine use in mental health. We mustn't forget that ketamine has saved countless lives, especially among veterans, first responders, autistic individuals, and young adults. In the face of the mental health crisis, healthcare professionals should unite, recognizing we're all in this together. Godspeed, Matt
References:
Malinovsky JM, Servin F, Cozian A, Lepage JY, Pinaud M. Ketamine and norketamine plasma concentrations after i.v., nasal and rectal administration in children. Br J Anaesth. 1996 Aug;77(2):203-7. doi: 10.1093/bja/77.2.203. PMID: 8881626.
Zanos P, Moaddel R, Morris PJ, Riggs LM, Highland JN, Georgiou P, Pereira EFR, Albuquerque EX, Thomas CJ, Zarate CA Jr, Gould TD. Ketamine and Ketamine Metabolite Pharmacology: Insights into Therapeutic Mechanisms. Pharmacol Rev. 2018 Jul;70(3):621-660. doi: 10.1124/pr.117.015198. Erratum in: Pharmacol Rev. 2018 Oct;70(4):879. PMID: 29945898; PMCID: PMC6020109.
Edwards, Johnathan. The Revolutionary Ketamine: The Safe Drug That Effectively Treats Depression and Prevents Suicide. Skyhorse publishing, 07-11-2023. https://www.amazon.com/Revolutionary-Ketamine-Effectively-Depression-Prevents-ebook/dp/B0BTZ6Q9KY?author-follow=B0C831QBX3
Eikermann M, Grosse-Sundrup M, Zaremba S, Henry ME, Bittner EA, Hoffmann U, Chamberlin NL. Ketamine activates breathing and abolishes the coupling between loss of consciousness and upper airway dilator muscle dysfunction. Anesthesiology. 2012 Jan;116(1):35-46. doi: 10.1097/ALN.0b013e31823d010a. PMID: 22108392; PMCID: PMC3246073.
Orhurhu VJ, Vashisht R, Claus LE, et al. Ketamine Toxicity. [Updated 2023 Jan 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541087/
Nakamura GR. Toxicologic assessments in acute heroin fatalities. Clin Toxicol. 1978;13(1):75-87. doi: 10.3109/15563657808988229. PMID: 367692.
Alex Berenson’s take on the situation …